For the embodiment of what has happened to the newspaper industry and to erstwhile good, hard-hitting investigative reporting, one need look no further than the Alexandria Town Talk.
It’s not that The Town Talk, one of five Gannett-owned newspapers in Louisiana and one of 123 Gannett publications in the U.S., Guam, and the United Kingdom, is necessarily the poster child for the fast-food media genre. But when a newspaper ignores a major news story all but gift-wrapped and dropped in its lap, it unavoidably becomes a microcosm for all that’s ailing the once robust medium.
So, what’s this big story that The Town Talk and other area media were repeatedly called about but chose not to pursue?
That would be the Veterans Administration Medical Center in Alexandria.
It’s not that the problems of veterans obtaining medical treatment from the VA has been hiding under a rock. It’s a national disgrace and it’s well documented that while the rest of the country is politely offering an empty, robotic “Thank you for your service” to our military, it begins to take on a hollow ring as our nation’s leaders continue to send our young men and women into harm’s way only to discard them when they return with missing limbs, closed head injuries, psychological disorders and PTSD. They’re quietly shunted aside and forgotten. The Pentagon, it seems, has little use for damaged merchandise—unless it’s a billion-dollar aircraft that won’t fly built by a defense contractor (read: campaign contributor) favored by some powerful member of Congress.
When a friend, a career soldier, was diagnosed with pancreatic cancer a few years ago, he was promptly discharged before he could qualify for his pension. Thank you for your service.
The horror stories of long waits for treatment and refusals of benefits and medication are by now well-known and it is no different at the Alexandria VA Medical Center.
But it is at that medical center that the stories become almost macabre in nature. And they all seem to revolve around a single doctor, Dr. Shivani Negi.
Here’s what we know about Dr. Negi:
- The families of several patients have signed affidavits attesting to her callous treatment of patients and her insistence that family members allow patients to die without attempts at resuscitation;
- Those same grief-laden affidavits describe in detail how abusive and non-communicative Dr. Negi becomes when families refused to sign “Do Not Resuscitate” (DNR) forms;
- Some family members said in their affidavits that they believed Dr. Negi allowed their loved ones to die deliberately and that she purposely removed them from the intensive care unit (ICU) to a remote room on another floor without benefit of one-on-one care normally given critical patients;
- Other doctors and nurses have provided written statements or testified in depositions as to her inappropriate remarks in the presence of family members and patients;
- The same doctors and nurses describe her violent temper and her threats to “kick butts” of subordinates;
The Commonwealth of Virginia granted her license to practice medicine after she testified she had never been refused a license elsewhere and that she had withdrawn her application in Florida. The only problem was Florida had actually refused her application a full two months prior to Virginia’s awarding her a license. Her Florida application, however, was not withdrawn until 2006.
The minutes of the Florida Board of Medicine’s Credential Committee of Sept. 13, 2003, provide little insight as to the reasons for the denial of her license application but do hint at some problem in Dr. Negi’s professional past.
“The applicant (Negi) was present and sworn in by the court reporters,” the minutes begin. “The applicant gave a brief history of events. The Committee discussed in length the seriousness of the issue. Dr. Tucker made a motion to deny the (application). The motion was seconded by Dr. Avila. The motion failed with Dr. Miguel, Dr. Davies and Mr. Dyches opposing. Dr. Davies made a new motion to deny the application…and allow 14 days to withdraw. The motion was seconded by Dr. Miguel. The motion passed unanimously.” 
The Florida statutes on which the application rejection was based were identical in both motions with only the provision to allow 14 days for Dr. Negi to withdraw added to the second motion.
There was no explanation of the “history of events” given by Negi, nor the circumstances of those “events.” Nor was there any explanation of the “issue” described deemed by the committee to be a serious sticking point in the consideration of her application.
The problem, however, could have been with the medical school she attended, Ross University School of Medicine (RUSM) in the Caribbean island nation of Dominica which was not accredited by the Association of American Medical Colleges, the body that approves medical programs in the U.S. as of September 2013, according to a story by Bloomberg Markets. http://www.bloomberg.com/news/articles/2013-09-10/devry-lures-medical-school-rejects-as-taxpayers-fund-debt
RUSM has since been taken over by Illinois-based DeVry University which Bloomberg says accepts students rejected by U.S. medical colleges. And even though it is a for-profit school, U.S. taxpayers pick up the tab for about 34 to 48 percent of students who default on their student loans which average about $250,000 compared to $170,000 for graduates of U.S. medical schools.
On her Florida application, a copy of which was obtained by LouisianaVoice, there were a series of questions and blocks to check for the appropriate “yes” or “no” answers.
For the question “Have you ever been dropped, suspended, placed on probation, expelled or requested to resign from any school, college or university,” she first checked “Yes” but scratched that answer out and checked “No.”
On another page further into her Florida application, she also checked “No” to the question: “Have you had any application for professional license or any application to practice medicine denied by any state board or other governmental agency of any state, territory, or country?”
Virginia apparently asks a similar question on its application forms because Dr. Negi submitted an “Addendum to questions 14 and 15” which said, “I had applied for a Florida license but changed my mind and did withdraw my application.” 
There is a problem with the timeline on that answer, however. LouisianaVoice has copies of a document from Florida Regulatory Specialist Cherise Davis which indicates Dr. Negi did not withdraw her application until June 8, 2006, nearly three years after her license was issued by Virginia.
In the case of Floyd Hamilton, Jr., a Bronze Star recipient who died in 2009, there are many questions but few answers.
Hamilton, 85 died at the hospital in 2009, nearly three years after Dr. Negi removed him from ICU to a room on another floor and far from the nurses’ station and without the ventilator support necessary, in the view of one physician who was involved in a verbal exchange with Dr. Negi when he attempted to treat Hamilton. Hamilton’s son claims his father suffered irreparable brain damage from the removal of the ventilator.
At least two other doctors at the VA hospital, as well as other staff members, have taken issue with both Dr. Negi’s medical decisions and her attitude toward patients and co-workers.
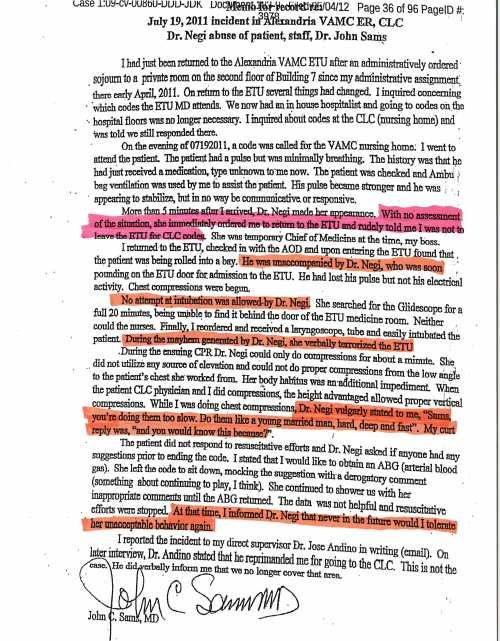
Dr. John Sams said he responded to a code for another patient on July 19, 2011, and found him “minimally breathing.” He initiated treatment and the patient’s pulse became stronger and he began to stabilize. 
“More than five minutes after I arrived, Dr. Negi made her appearance,” he wrote in his signed report. “With no assessment of the situation, she immediately ordered me to return to the (Express Treatment Unit) and rudely told me I was not to leave the ETU for CLC (Community Living Center, or VA nursing homes) codes. She was temporary Chief of Medicine at the time, my boss,” he wrote.
“I returned to ETU…and upon entering found that the patient was being rolled into a bay. He was unaccompanied by Dr. Negi, who was soon pounding on the ETU door for admission. He (Hamilton) had lost his pulse. Chest compressions were begun.
“No attempt at intubation was allowed by Dr. Negi. Finally, I reordered and received a laryngoscope tube and easily intubated the patient. During the mayhem by Dr. Negi, she verbally terrorized the ETU. While I was doing the chest compressions, Dr. Negi vulgarly stated to me, ‘Sams, you’re doing them too slow. Do them like a young married man—hard, deep and fast.’”
Dr. Sams wrote that Hamilton did not respond to resuscitative efforts and Dr. Negi “asked if anyone had any suggestions prior to ending the code.” Sams said he said he would like to obtain an arterial blood gas (ABG)—a procedure to determine how well the lungs are moving oxygen into the bloodstream. “She left the code to sit down, mocking the suggestion with a derogatory comment. She continued to shower us with her inappropriate comments until the ABG returned. The date was (sic) not helpful and resuscitative efforts were stopped. At that time, I informed Dr. Negi that never in the future would I tolerate her unacceptable behavior.”
Dr. Sams said he reported the incident in writing to his director supervisor who, instead of taking action against Dr. Negi, reprimanded Sams for responding to the CLC code.
Dr. Mark St. Cyr, an emergency room contract physician, testified in a deposition that he had a conflict with Dr. Negi from the first moment they met. He said Dr. Negi threatened to “kick my butt” after he sought permission to admit an ER patient into the hospital. His deposition was given in a lawsuit by Floyd Hamilton, III, the deceased patient’s son.
He said the younger Hamilton gave specific instructions that he wanted his father kept in ICU and that the family “wanted everything possible done” to keep his father alive—and that he did not wish to sign a Do Not Resuscitate (DNR) order.
Attorney Robert Evans, III, indicated in the deposition of Dr. St. Cyr that he had been in communication with the families of several patients of Dr. Negi “who believe that their family members have died from her treatment.” 
Floyd Hamilton, III, as did family members of other patients, said Dr. Negi became incensed and abusive when her requests for DNR orders were not signed by family members. Hamilton said she even stopped communicating with him and would not return his calls.
Documents showed that Dr. Negi even sent a $50 money order to one woman in Leesville so that she could travel to Alexandria to sign a DNR order.
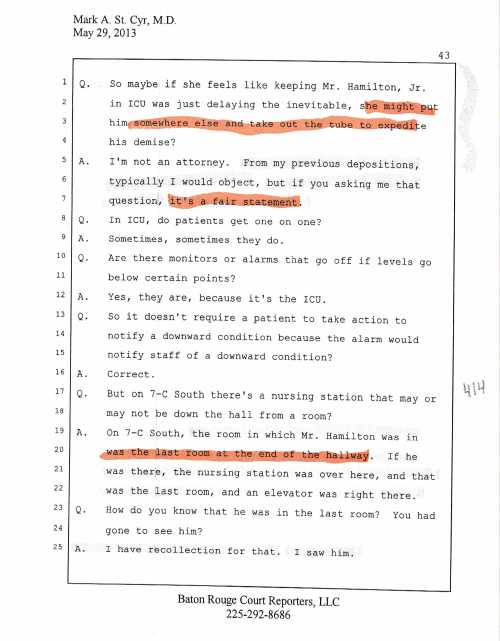
Dr. St. Cyr said Dr. Negi’s decision to remove a tube protecting his airway was not consistent with the family’s wishes. Asked in his deposition of removing the tube was not consistent with the family’s request to do everything possible, Dr. St. Cyr responded, “That’s a fair statement.” 
St. Cyr described Dr. Negi as “aggressive” in terms of “getting patients in and getting them out” of the hospital. “(If) she doesn’t feel like something is worth it, she may not be quite as aggressive medically in terms of performing certain actions,” he said.
When asked by attorney Evans if “she might put him somewhere and take out the tube to expedite his demise,” Dr. St. Cyr again replied, “It’s a fair statement.” 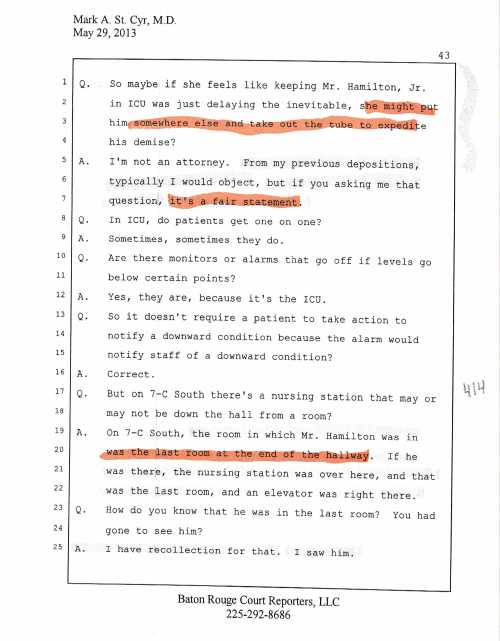
That line of questioning developed over St. Cyr’s description of how Dr. Negi removed the elder Hamilton from ICU to another floor at the end of a hall furthest from the nurses’ station. “Why would he (Hamilton) go to the floor, the last room at the end of the hallway (when he) can’t press a button, can’t call a nurse, or anything, and he’s not even responsive?” he asked. “You’re literally putting the person out there to die.”
Asked if any other hospital personnel were involved in the removal of the intubation of Hamilton, Dr. St. Cyr said, “No, sir. That’s solely Dr. Negi. When a person’s in the intensive care unit, Dr. Negi was in charge and you don’t go against Dr. Negi.”
Two nurses also filed written reports of the confrontation involving Dr. Negi and Dr. Sams, both claiming that Dr. Negi was yelling, belligerent, unprofessional, and throwing her gloves. “…She stated, ‘You never stop CPR,’” one of the nurses quoted her as saying. “CPR was never stopped on the vet other than when Dr. Negi was doing CPR.” The same nurse said Dr. Negi “continued to berate Dr. Sams” because Dr. Sams wanted a blood gas. Dr. Negi made the comment to respiratory, ‘Well I guess you will get to practice your collection of blood gases.’”
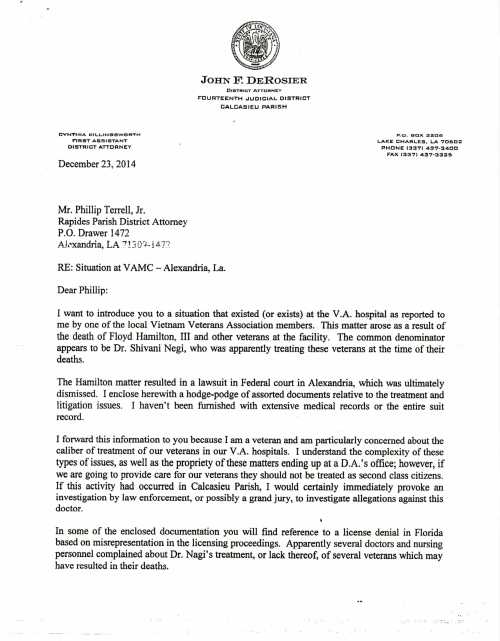
The Calcasieu Parish District Attorney, in a letter to his counterpart in Rapides, intimated that had the events involving Hamilton occurred in Calcasieu, “I would certainly immediately provoke an investigation by law enforcement, or possibly a grand jury, to investigate allegations against this doctor.”
D.A. John Derosier, in his Dec. 23, 2014, letter to Rapides D.A. Phillip Terrell, Jr., wrote, “Please have someone…determine whether or not there is sufficient basis to move forward with a formal investigation.”
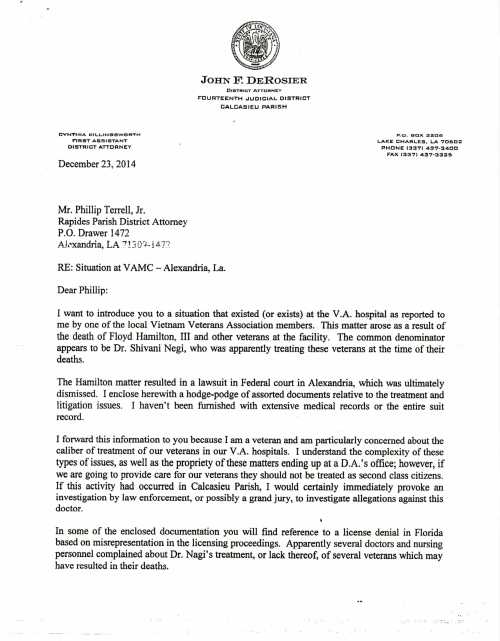

Terrell, claiming his office was not equipped for such an extensive investigation, asked for assistant from then-Attorney General Buddy Caldwell’s office and Assistant Attorney General Arthur Ogea of Lake Charles was given the assignment.
Jeff Landry, upon taking office as Caldwell’s successor, however, fired Ogea and seized all his records on the Hamilton case. Contacted by LouisianaVoice, Ogea agreed to talk in more detail about his thoughts in the coming days but did say he felt there was sufficient evidence for a grand jury investigation and possible charges of negligent homicide against Negi.
It will be interesting to see how Louisiana’s new attorney general proceeds with this investigation.
Floyd Hamilton, III, meanwhile, kept applying pressure by picketing the hospital and by notifying members of Louisiana’s congressional delegation and VA officials.
Because he took photographs of his father that showed the stark contrast between the elder Hamilton’s condition before and after being removed from ICU, there is now a sign posted at the VA Hospital in Alexandria proclaiming an absurd—and unenforceable—rule that photographs are no longer allowed at the facility.
The Department of Veterans Affairs, Office of Inspector General, conducted an investigation of “suspicious deaths” at the Alexandria VA hospital. In its executive summary dated Feb. 14, 2008, the OIG repeatedly—and predictably—said that investigators “did not substantiate” any of the allegations involving Hamilton or any of several other patients who died while in the care of Dr. Negi.
Five days later, Christina Lavine, director of the VA’s Hotline Division, wrote Hamilton’s son, Floyd Hamilton, III to say that the VA OIG had closed his father’s case. “As we advised you when we opened this case, our decision to close a Hotline case is final, and there are no appeal rights,” she wrote.
Instead of definitive, meaningful action, all we’re received so far are insincere apologies and empty promises that conditions will improve. But they never do.
A congressional subcommittee held hearings on the Alexandria VA Hospital only last week. Even though subcommittee members were well aware of irregularities pointed out by Floyd Hamilton, III, and even though he was in attendance at the hearing, he was never allowed to testify. Perhaps, to borrow a phrase from Al Gore, Hamilton’s claims constituted “an inconvenient truth” to officials who should be infuriated at the manner in which our veterans are treated upon their return from duty.
Read Full Post »